Spinal Fusion: A Patient’s Guide to Surgery, Recovery, and Renewed Strength
Are you a candidate for a spinal fusion procedure? We’ll tell you what you need to know and how best to prepare for the surgery.
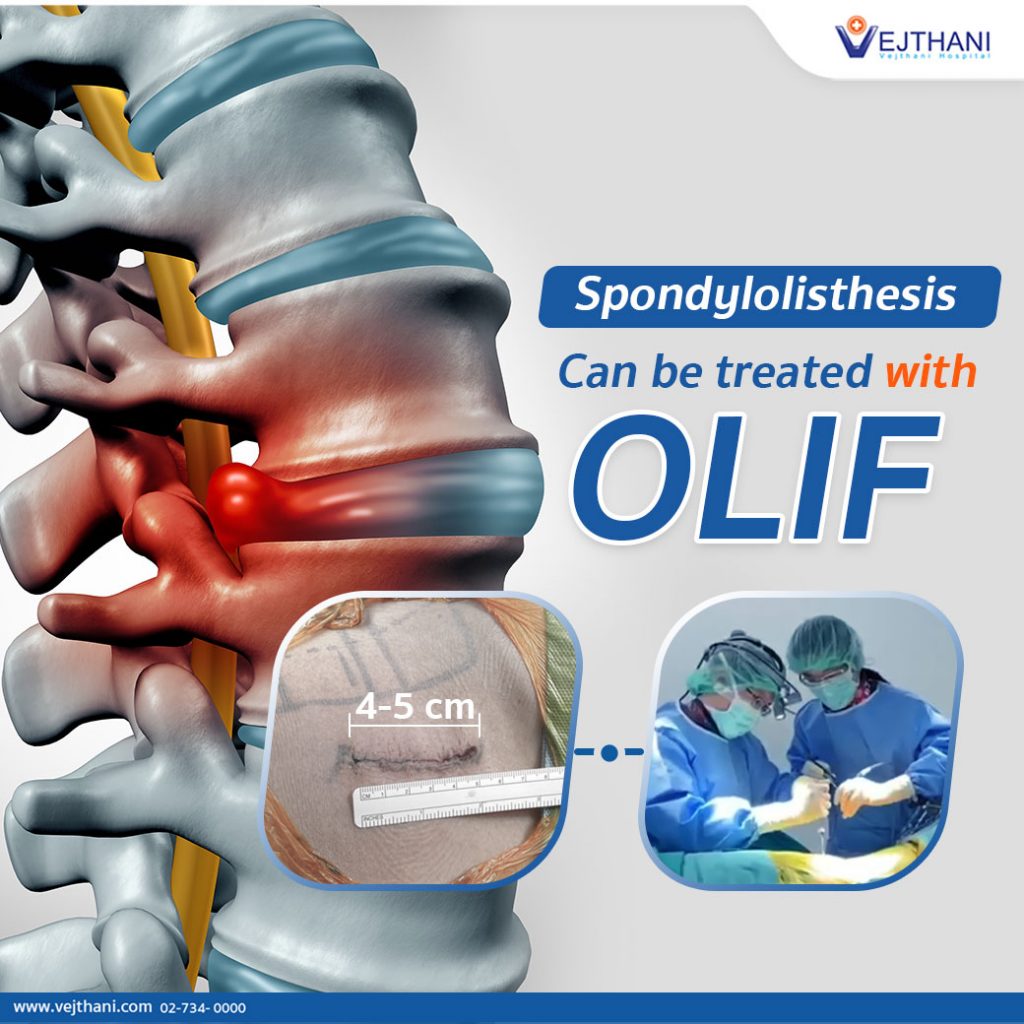
Having difficulties walking and severe back pain that radiates down to the legs may be a sign of Spondylolisthesis. Spondylolisthesis can occur in people of all ages, but this condition can be permanently treated with spinal fusion surgery called Oblique Lumbar Interbody Fusion (OLIF). Patients can often get back on their feet within 12 – 24 hours after the surgery.
Spondylolisthesis is a spinal condition that causes severe pain. Both elderly and adolescents can experience the condition.
Patients with Spondylolisthesis have primary symptoms that include pain when bending or arching their back which radiates down to the legs, and numbness in one or both legs. Aside from these symptoms, Spondylolisthesis can also cause tightness or stiffness in the lower back, especially in the hips and thighs. Moreover, additional symptoms include leg muscle weakness that causes difficulties walking or an inability to walk long distances. These symptoms will usually persist longer than 2 weeks until it greatly impacts the patient’s daily life.
Spondylolisthesis is caused by a rupture or severe damage to the spinal disc (intervertebral discs) that causes the fluid in the discs to leak or slip out of place and compress the nerves. The spinal discs are located in between each vertebrae of the spinal cord. They are made up of jelly-like substances that work as shock absorbers to support the weight transmitted through the spine and help it to move. The intervertebral discs can be easily damaged or torn when the spine is heavily used or injured and it may require spinal fusion surgery to ease pain and restore normal movement.
There are two primary causes of Spondylolisthesis. The first one usually occurs in the elderly, and is often caused by degeneration of the spinal column in the joints and in the spinal discs that lead to an unstable spine, resulting in the vertebrae slipping out of place and compressing the nerves. The second one occurs in younger people and is generally caused by Spina Bifida, a spine condition that is apparent at birth or results from a severe spinal injury. However, lifestyle can also be a factor that causes Spondylolisthesis. For instance, being overweight, regularly lifting heavy things, having an incorrect sitting posture, sudden erratic movements, and playing extreme sports that directly affect the spine are the stimulators behind Spondylolisthesis
For the diagnosis and treatment of Spondylolisthesis, the doctor will start by determining the cause. A physical examination, X-rays and MRI scans are used to examine the severity of the disease. If the condition is mild, the doctor will treat the patient by prescribing medication along with physiotherapy for around 6 – 8 consecutive weeks. However, if the symptoms do not improve or become severe to the extent where it is affecting the patient’s daily life, the doctor will recommend a disc replacement surgery. If the patient has a spine deformity or scoliosis, the doctor may consider performing the Oblique Lumbar Interbody Fusion (OLIF). This is a minimally invasive spinal fusion surgery. The procedure consists of a small incision made on the side of the body to replace the damaged disc with an artificial disc and restore the spinal alignment and nerve compression with the lumbar fusion peek cages. This spinal fusion surgery results in small incisions and reduces the damage to nearby tissues and muscles, reduces blood loss, and the risk of complications as well as nerve injury. In addition, it lowers the risk of post-operative membrane in the nerves. Patients will be able to get back on their feet within 12 – 24 hours after the spinal fusion surgery and most importantly, the recovery period is only 1 night of admission at the hospital.
Spine Center, Vejthani Hospital
Call 02-7340000 or Ext. 5500
English Hotline: (+66)8-522 38888