Diabetic foot ulcer occurs in numerous diabetic patients, and oftentimes they end up with lower limbs amputation. Complication related to diabetic foot is one of the major reasons behind long term hospitalizations. Not only it is beneficial for patients to be informed of the ways to prevent foot ulcer from an early stage, but it is vital to take extra care before the sign appears. After all, one of the best treatment methods for foot ulcers is to stop the wound from developing or spreading further.
Diabetic foot ulcer is an open wound or sore mostly found on the bottom of the foot. It becomes extremely concerning when patients with diabetic neuropathy especially with foot numbness, experience foot injury. Because they are unable to feel any pain or abnormal signs. That injury is the main trigger point that can lead to foot ulcers.
Follow these measures and cares to prevent foot ulcers from occurring.
- Examine your feet regularly. Pay attention to in-between toes. Look for blisters, thickened, discoloration, cracking, swelling, irritation, torn skin, or open wounds.
- Cleanse your toenails daily. Make sure to dry them well.
- Take extra care of your feet. Do not walk barefoot or wear shoes without socks that could expose your feet to splinters, sand or concrete. These can cut or bruise your skin.
- Wear well-fitting and soft sole shoes. Hard soles, too tight or too loose footwear can be harmful.
- Maintain your blood sugar and cholesterol levels. High lean protein and fiber diets can help manage your diabetes. Avoid eating meals that are high in saturated fats. Minerals like iron, zinc, and copper contain components that help accelerate cell growth and connective tissues in the body.
Following these 5 measures can reduce the chances of having diabetic foot ulcers, but what are the precautions you should take to prevent existing foot ulcers from getting infected?
- Strictly control your blood sugar level
- Keep the ulcer or the wound clean and covered with bandage
- Daily wound dressing to clean the ulcer
- Do not walk barefoot when your foot has a wound
Being aware of the preventing guidelines is important but itself alone may not be enough to reduce the chance of developing diabetic foot ulcer. Knowing the characteristics of people who are prone to foot ulcers will lead to better prevention.
Patients who suffer from neuropathy, poor blood circulation, foot deformity, or uncontrolled diabetes are at high risk. Additional factors include smoking, drinking alcohol, putting heavy pressure or friction on the feet.
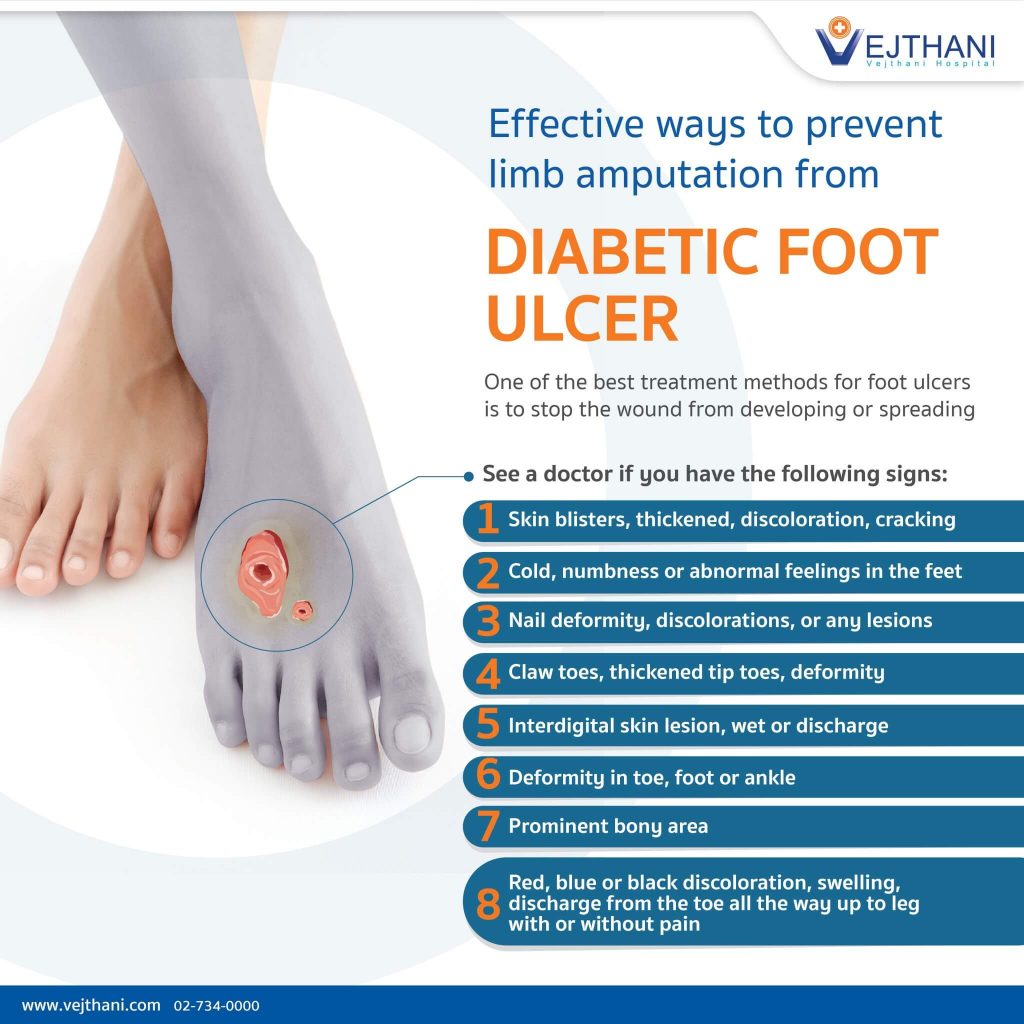
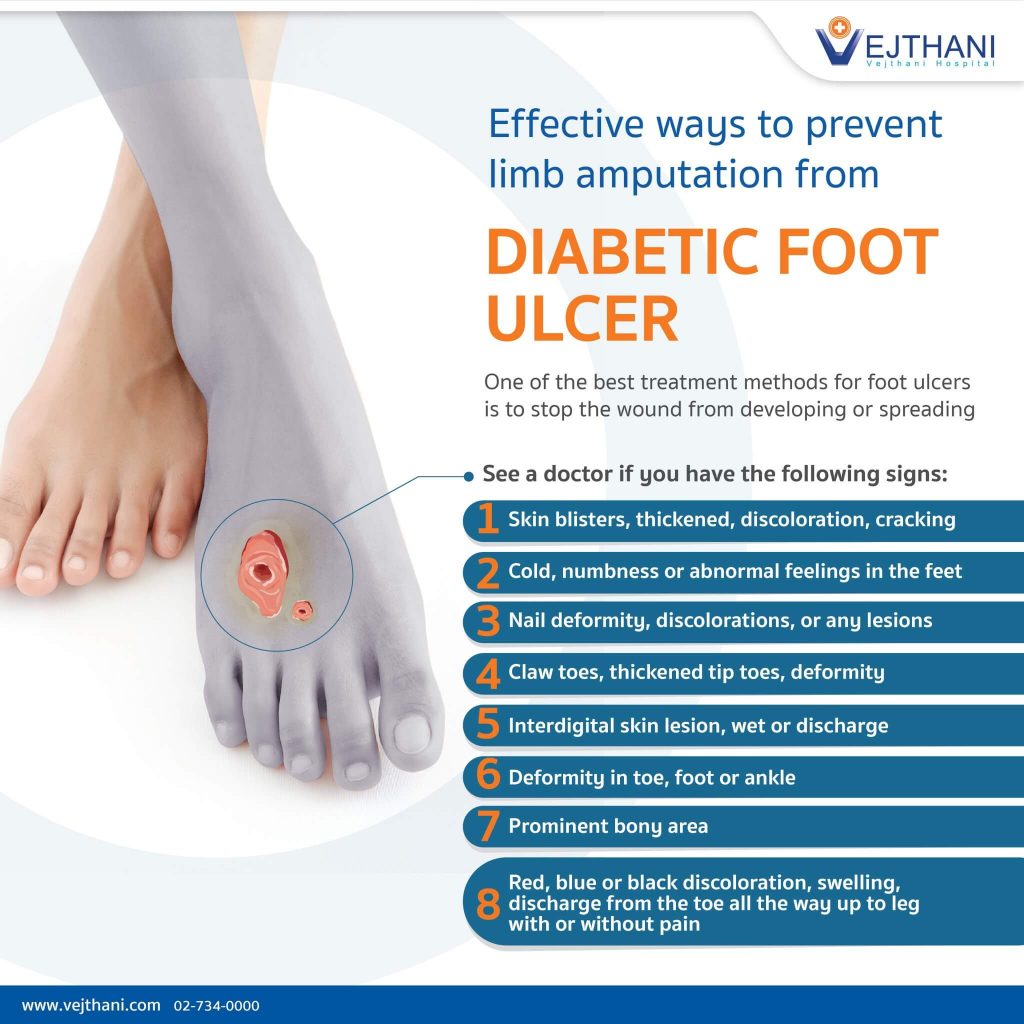
When to see a doctor?
In the event of having these lesions or concerning signs, consult your doctor immediately. Because these may result in diabetic foot ulcer.
- Skin blisters, thickened, discoloration, cracking
- Cold, numbness or abnormal feelings in the feet
- Nail deformity, discolorations, or any lesions
- Claw toes, thickened tip toes, deformity
- Interdigital skin lesion, wet or discharge
- Deformity in toe, foot or ankle
- Prominent bony area
- Red, blue or black discoloration, swelling, discharge from the toe all the way up to leg with or without pain
Your podiatrist will determine if you are at high risk of getting foot ulcer. Overlooking of a slight abnormality could be harmful.
Early detection of diabetic foot ulcer is the best preventive measure for limb amputation.
Contact Diabetic Foot and Wound Center at Vejthani Hospital on 3rd floor or call +66(0)85-223-8888 Hotline for more information.
- Readers Rating
- Rated 3.6 stars
3.6 / 5 ( Reviewers) - Very Good
- Your Rating