What is Varicose Veins?
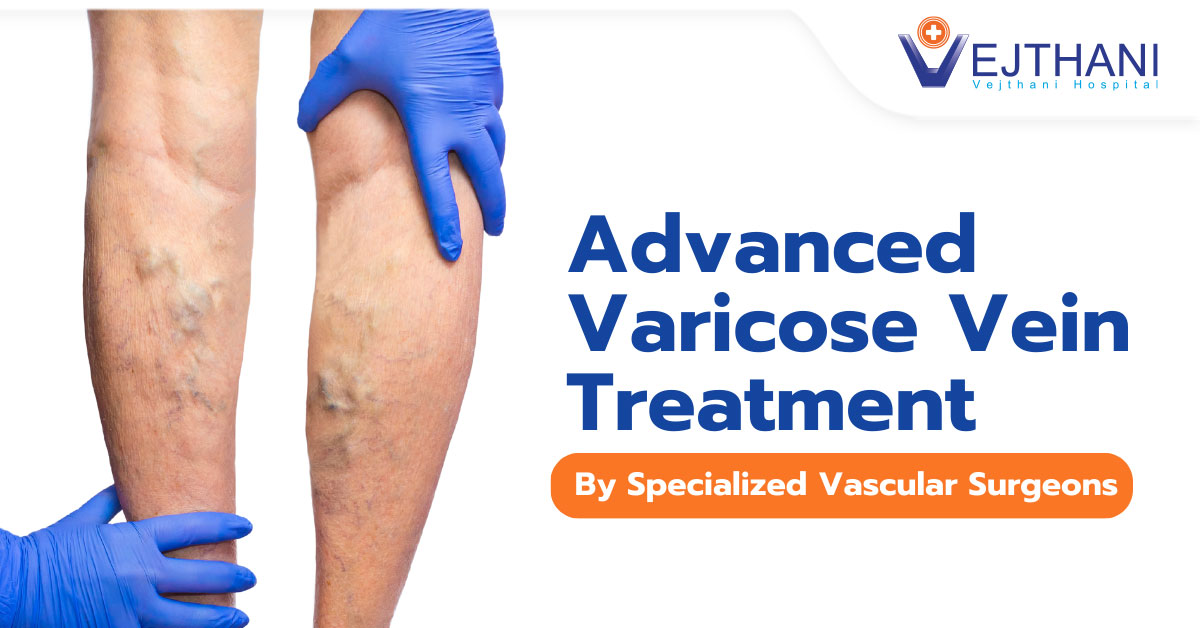
Varicose veins occur when veins have become enlarged and twisted; they appear bulged and swollen. Veins close to the skin’s surface (superficial) are likely to develop into varicose veins. The legs are most commonly affected by varicose veins, as standing and walking increases pressure in the veins of the lower body.
While many consider varicose and spider veins mild variations of varicose veins and a cosmetic concern, they can also be a source of aching pain and discomfort for others. Sometimes, varicose veins may lead to more severe complications. Treatment may include self-care measures or medical procedures to close or remove the affected veins.
Typically found on the legs, these veins are visible through the skin and are often accompanied by spider veins. Varicose veins are not confined solely to the surface; they may develop deeper beneath the skin, escaping easy visibility. This hidden manifestation of vein disease tends to worsen over time. Hence, it is crucial for vascular specialists to delve beneath the surface to address the underlying cause effectively.
While many consider varicose and spider veins mild variations of varicose veins and a cosmetic concern, they can also be a source of aching pain and discomfort for others. Sometimes, varicose veins may lead to more severe complications. Treatment may include self-care measures or medical procedures to close or remove the affected veins.
Typically found on the legs, these veins are visible through the skin and are often accompanied by spider veins. Varicose veins are not confined solely to the surface; they may develop deeper beneath the skin, escaping easy visibility. This hidden manifestation of vein disease tends to worsen over time. Hence, it is crucial for vascular specialists to delve beneath the surface to address the underlying cause effectively.
What Causes Varicose Veins?
Varicose veins may result from weakened or impaired valves. Imagine a river flowing uphill. While arteries carry blood from the heart to the body, veins are crucial in returning blood from the body to the heart. The veins in the legs face the challenge of working against gravity to transport blood from the body to the heart.
When this happens, the lower leg muscles contract, serving as effective pumps, and the elastic walls of the veins help guide the blood back to the heart. To make this happen, tiny valves within the veins open as blood moves towards the heart and quickly closes to prevent any backward flow. However, if these valves are weak or damaged, blood can flow backward, accumulating blood in the veins. This causes the veins to stretch or twist, eventually leading to the development of varicose veins.
When this happens, the lower leg muscles contract, serving as effective pumps, and the elastic walls of the veins help guide the blood back to the heart. To make this happen, tiny valves within the veins open as blood moves towards the heart and quickly closes to prevent any backward flow. However, if these valves are weak or damaged, blood can flow backward, accumulating blood in the veins. This causes the veins to stretch or twist, eventually leading to the development of varicose veins.
Who is at Risk of Developing Varicose Veins?
- Increased age: Aging causes valves in the veins that control blood supply to wear off. That leads to some blood flow backwards into the veins.
- Gender: Women are more susceptible to developing varicose veins due to hormonal changes before menstruation or during pregnancy or menopause, as the female hormones relax the vein walls. Also, hormone treatments like the intake of birth control pills may pose the risk of developing varicose veins.
- Pregnancy: Pregnancy increases blood volume in the body, leading to enlarged veins in the legs.
- Genetics: Familial history is a significant risk factor.
- Excess weight: Obesity puts additional pressure on veins.
- Prolonged standing or sitting: Lack of movement hinders blood flow. Sitting or standing for long periods, especially in positions restricting blood flow, such as crossing your legs, walking, or standing in high heels.
Signs and Symptoms of Varicose Veins
- Dark purple or blue veins
- Veins with a twisted and bulging appearance, resembling cords on the legs.
- Aching or sensations of heaviness in the legs
- Burning, throbbing, muscle cramping, and swelling in the lower legs
- Increased pain after prolonged periods of sitting or standing
- Itching around the veins
Management of varicose veins involves self-care practices, the use of compression stockings, as well as surgical or procedural interventions. Typically, treatments for varicose veins are conducted on an outpatient basis, allowing you to return home the same day. Moreover, advanced minimally invasive treatments are available, ensuring a swift and smooth recovery process.
What are the Treatments offered at Vejthani Hospital?
1. Sclerotherapy
Sclerotherapy sits at the forefront of treatments for varicose veins, ensuring complete and lasting results. However, starting with sclerotherapy for spider veins without addressing underlying venous insufficiency can be a misstep. Some varicose veins have a hidden culprit: deeper larger veins that feed those varicose veins. By removing these larger veins, the smaller ones often disappear naturally. This approach prioritizes the root cause. Any remaining varicose veins can then be effectively treated with sclerotherapy.
Sclerotherapy is performed by injecting a small amount of a liquid chemical solution into spider veins using a tiny needle. This causes the veins to harden, preventing them from filling with blood. Over time, the injected veins will shrink and fade as the body naturally absorbs the scar tissue. The solution induces scarring, closes off abnormal veins, and seals them off from healthy veins. Treated veins undergo shrinkage and are subsequently absorbed by the body. For larger varicose veins, the chemical solution can be more beneficial when administered in foam form instead of liquid. This specialized procedure, known as foam sclerotherapy, applies to deeper veins done by ultrasound guidance. Sclerotherapy doesn’t require anesthesia. You should be able to walk and resume work promptly after undergoing the procedure, and it is recommended that you wear compression stockings for a month.
2. Endovenous Treatment
If endovenous ablation treatments and sclerotherapy do not work, the recommendation would be a surgical intervention known as high ligation and vein stripping to remove the affected veins. The surgery is performed under general anesthesia, ensuring that you remain asleep throughout the procedure. Ligation is done by tying off a vein before it connects to a deep vein, and the vein is then extracted through small incisions. The first incision, approximately 5cm, is made near the groin at the top of the varicose vein. The second, smaller incision is positioned lower down the leg, typically around your knee. The vein near the groin, is secured and sealed. A slender, flexible wire is threaded through the lower part of the vein and carefully drawn out through the lower incision in the leg. It’s important to note that the surgery does not impact blood flow in the legs. The deeper veins within the legs will seamlessly take on the role of the compromised veins.
Sclerotherapy is performed by injecting a small amount of a liquid chemical solution into spider veins using a tiny needle. This causes the veins to harden, preventing them from filling with blood. Over time, the injected veins will shrink and fade as the body naturally absorbs the scar tissue. The solution induces scarring, closes off abnormal veins, and seals them off from healthy veins. Treated veins undergo shrinkage and are subsequently absorbed by the body. For larger varicose veins, the chemical solution can be more beneficial when administered in foam form instead of liquid. This specialized procedure, known as foam sclerotherapy, applies to deeper veins done by ultrasound guidance. Sclerotherapy doesn’t require anesthesia. You should be able to walk and resume work promptly after undergoing the procedure, and it is recommended that you wear compression stockings for a month.
2. Endovenous Treatment
2.1 Thermal ablation
This procedure is conducted under either local or general anesthesia. During post-procedure, you might experience some tightness in your legs, and the treated areas may be bruised and painful. While nerve injury is a potential risk, it is typically temporary.
2.1 Non-thermal ablation I VenasealTM venous closure procedure Venaseal procedure offers a minimally invasive solution for varicose veins, eliminating the need for cuts or needles. Using ultrasound imaging, the doctor will insert a catheter into the vein and guide it into the correct position. Then delivers a small amount of specially formulated medial adhesive to seal or close the diseased vein, rerouting blood to nearby healthy veins, which provides symptom relief. The ultrasound helps ensure closure of the entire length. This procedure is a 30 to 60 minutes outpatient procedure that can be performed on both legs with minimal pain and requires no tumescent anesthesia. Typically, patients return to normal activity on the same day as their procedure.
3. High Ligation and Vein Strippin
I Radio Frequency Ablation Therapy (EVRFA)
Endovenous Radio Frequency Ablation Therapy (EVRFA)is a minimally invasive treatment with fewer risks of complications. It is done by heating the wall of a varicose vein using radiofrequency energy. This treatment relieves the symptoms and targets the underlying condition that causes varicose veins. A small incision is made for a thin catheter to enter your vein near the knee, guided by ultrasound imaging. Injecting local anesthesia around the vein serves a dual purpose: it isolates the vein from surrounding tissues and subsequently numbs the targeted area. Once the anesthesia has taken effect within the vein, the radiofrequency is activated, initiating the process of heating (ablation) the vein from the inside. This heat causes the vein wall to collapse and seal shut, naturally redirecting blood flow to healthier veins. You will then need to wear a compression stocking or wrap your leg with a multilayer compression bandage, which you should consistently wear for the first 48 hours and then daily for the subsequent 2 weeks (excluding nighttime use). Walking and resuming work is possible immediately after the procedure. Endovenous Radio Frequency Ablation Therapy targets the deeper, larger veins contributing to varicose veins, offering a more comprehensive solution.
II Endovenous Laser treatment (EVLA) Endovenous laser treatment offers a minimally invasive solution for varicose veins, eliminating the need for cuts or needles. Using ultrasound imaging, the doctor will insert a catheter into the vein and guide it into the correct position. A tiny laser positioned at the top of the varicose vein will deliver precise bursts of light energy to heat up, the laser gently targets the vein and seals it closed, causing it to gradually fade and disappear over time. The ultrasound helps ensure closure of the entire length.
II Endovenous Laser treatment (EVLA) Endovenous laser treatment offers a minimally invasive solution for varicose veins, eliminating the need for cuts or needles. Using ultrasound imaging, the doctor will insert a catheter into the vein and guide it into the correct position. A tiny laser positioned at the top of the varicose vein will deliver precise bursts of light energy to heat up, the laser gently targets the vein and seals it closed, causing it to gradually fade and disappear over time. The ultrasound helps ensure closure of the entire length.
This procedure is conducted under either local or general anesthesia. During post-procedure, you might experience some tightness in your legs, and the treated areas may be bruised and painful. While nerve injury is a potential risk, it is typically temporary.
2.1 Non-thermal ablation I VenasealTM venous closure procedure Venaseal procedure offers a minimally invasive solution for varicose veins, eliminating the need for cuts or needles. Using ultrasound imaging, the doctor will insert a catheter into the vein and guide it into the correct position. Then delivers a small amount of specially formulated medial adhesive to seal or close the diseased vein, rerouting blood to nearby healthy veins, which provides symptom relief. The ultrasound helps ensure closure of the entire length. This procedure is a 30 to 60 minutes outpatient procedure that can be performed on both legs with minimal pain and requires no tumescent anesthesia. Typically, patients return to normal activity on the same day as their procedure.
If endovenous ablation treatments and sclerotherapy do not work, the recommendation would be a surgical intervention known as high ligation and vein stripping to remove the affected veins. The surgery is performed under general anesthesia, ensuring that you remain asleep throughout the procedure. Ligation is done by tying off a vein before it connects to a deep vein, and the vein is then extracted through small incisions. The first incision, approximately 5cm, is made near the groin at the top of the varicose vein. The second, smaller incision is positioned lower down the leg, typically around your knee. The vein near the groin, is secured and sealed. A slender, flexible wire is threaded through the lower part of the vein and carefully drawn out through the lower incision in the leg. It’s important to note that the surgery does not impact blood flow in the legs. The deeper veins within the legs will seamlessly take on the role of the compromised veins.
Does Compression Stockings help treat Varicose Veins?
The initial course of action often involves wearing compression stockings throughout the day. These stockings exert pressure on the legs, helping blood flow in the leg more efficiently. The degree of compression varies depending on the type and brand of stockings. It’s essential to note that compression stockings are not a cure for varicose veins. They can help manage the symptoms and prevent the condition from getting worse. If varicose veins are causing symptoms, prescription-strength stocking is an option.
How is Varicose Vein Diagnosed?
Vericose vein is diagnosed by physical examination and imaging procedures. The doctor may perform a physical examination by observing the legs while the patient is standing to look for swelling. The patient will be asked to describe any pain or aching sensations in the legs. To confirm the diagnosis and understand the root cause, a venous Doppler ultrasound of the leg is done. This non-invasive test utilizes sound waves to analyze blood flow in the leg veins, providing insights into the structure of the veins and detecting the presence of any blood clots.
Complications of Varicose Veins are uncommon but can be found in some cases:
- Ulcers: Painful ulcers can appear on the skin close to the varicose veins, especially around the ankles. It may start with a discolored spot on the skin. If you suspect the development of a leg ulcer, seek immediate medical attention.
- Blood clots: Sometimes, deeper veins in the legs can become enlarged, resulting in pain and swelling. Continuous pain or swelling should prompt medical attention as it could signify the presence of a blood clot.
- Bleeding: There are instances where veins close to the skin may rupture. While this typically results in minor bleeding, it needs medical intervention.
What can you do to Prevent?
Enhancing blood flow and muscle tone could decrease the likelihood of developing varicose veins. Following measures that alleviate discomfort from varicose veins can also serve as preventive actions. Consider the following:
- Avoid wearing high heels and tight hosiery
- Frequently changing your sitting or standing position
- Adhere to a high-fiber, low-salt diet
- Engage in regular exercise
- Elevate your legs when sitting or lying down
- Monitor and maintain a healthy body weight
Vejthani Hospital stands prepared to address varicose veins at every stage. Our team of specialists, armed with cutting-edge technology, including thermal injections, high-frequency radio waves, and surgical interventions. Our compassionate team will listen to your concerns, assess your condition, and recommend the most suitable treatment plan, ensuring you achieve optimal results with minimal discomfort and downtime.
- Readers Rating
- Rated 5 stars
5 / 5 ( Reviewers) - Spectacular
- Your Rating