
Arteriovenous fistula
Overview
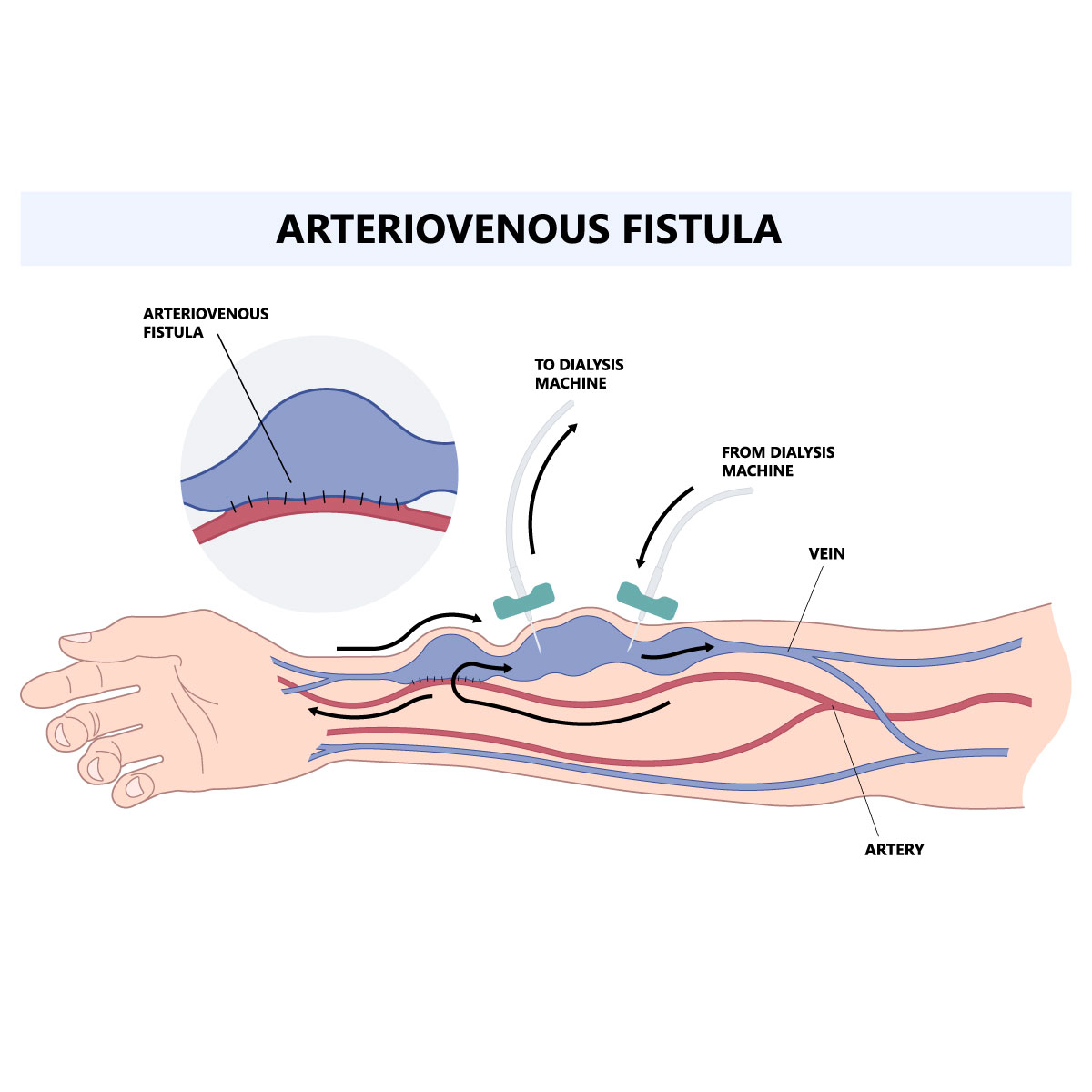
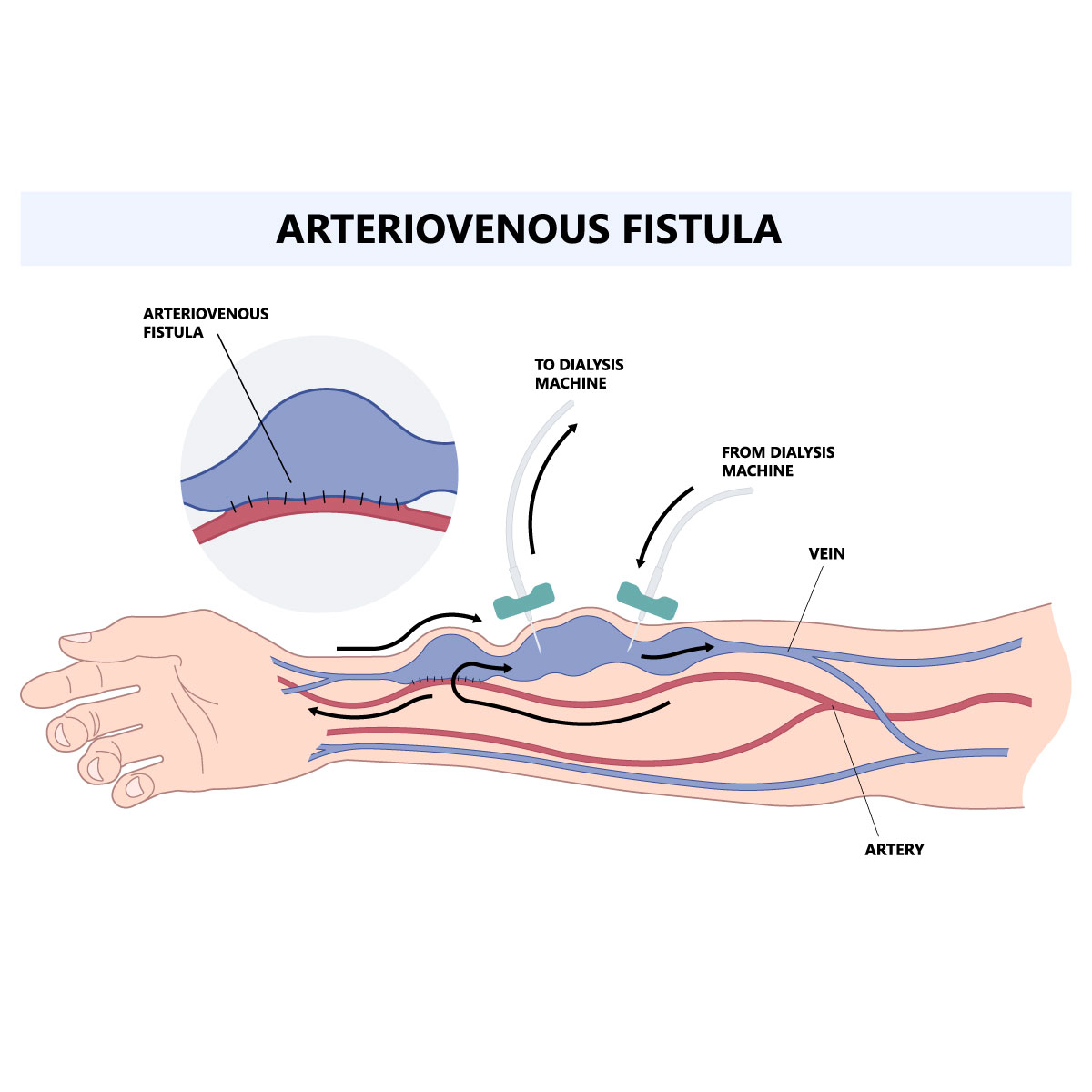
Arteriovenous fistula is an abnormal connection between an artery and a vein that allows blood to flow in the opposite direction, avoiding the capillaries and resulting in less blood reaching the tissue below them. Normally, the capillaries receive blood from the arteries and deliver it to the veins. Oxygen and nutrients are carried to the body’s tissues by capillaries.
Fistulas can range from being harmless (or even useful when there is a medical need to generate one, for some cases it is created for people with severe kidney disease to help them with dialysis), to being a serious health problem that permanently harms the heart, depending on where they are, how they formed, and their size. Although it could affect any parts of the body where an artery and a vein connect, it commonly affects the legs.
The location of an arteriovenous fistula in the body affects the symptoms and may lead to serious consequences if left untreated. Arteriovenous fistulas can be treated with monitoring, compression, catheter-based techniques, and occasionally surgery.
The abnormal connections between an artery and a vein that covers over the brain or spinal cord are known as dural arteriovenous fistulas (dAVFs) and are a type of arteriovenous fistula that can develop in the brain, spinal cord, or other parts of your body.
Symptoms
There are frequently no symptoms or signs associated with small arteriovenous fistulas in the arms, legs, lungs, kidneys, or brain. The normal course of treatment for small arteriovenous fistulas is observation by a specialist. Symptoms and signs of large arteriovenous fistulas may develop depending on which part is affected.
Signs and symptoms of an arteriovenous fistula include:
- Swelling surrounding the fistula’s site is most likely to occur when the fistula is directly below the skin. Mostly at the arms and legs.
- Bulging, purple veins that are visible through the skin and resemble varicose veins.
- Gastrointestinal bleeding if the fistula is located at the digestive tract
- Fatigue
- Heart failure
- Lower blood pressure
Pulmonary arteriovenous fistula, which is a large arteriovenous fistula in the lungs, it is a serious condition that can result to:
- Lack of blood flow might result in pale gray or blue lips or fingernails (cyanosis)
- Coughing up blood
- Widening and atypically rounded fingertip appearance (clubbing)
Arteriovenous fistulas may be more easily treated if they are discovered early and will reduce the risk of complication such as blood clot and heart failure. If you notice these symptoms, consult your doctor.
Causes
Congenital (existing at birth) or acquired (occurring later in life) arteriovenous fistulas are both possible. Arteriovenous fistulas may be caused by:
- Injury: Arteriovenous fistulas are most frequently unintentionally caused by trauma. As a results from penetrating injuries such as gunshot or stab wound that damages to an adjacent artery and vein.
- Congenital: Develop while the child is in the womb, in which instead of a single, larger fistula, they typically involve a number of smaller ones. If they occur in a dangerous area, some are fatal.
- Dialysis: The most frequent cause of arteriovenous fistulas in patients undergoing dialysis. An arteriovenous fistula aids in the development of a thicker, larger vein that can carry more blood into and out of your body and is suited to withstand dialysis needles and high pressure.
- Genetic conditions: results in abnormal blood vessels throughout the body, particularly in the lungs, it can produce pulmonary arteriovenous fistulas, which are those located in the lungs. Osler-Weber-Rendu disease, also referred to as hereditary hemorrhagic telangiectasia, is one of these conditions.
Risk factors
Fistulas are very common and a certain sort is more prevalent in some populations, typically because of their personal circumstances. Arteriovenous fistulas are more likely to develop in certain genetic or congenital abnormalities exist. The following are additional potential risk factors for arteriovenous fistulas:
- Age: common as the person grows older.
- Gender: common among female than male.
- Procedure: an operation involving groin blood vessels such as cardiac catheterization.
- Medications: such as various blood thinners (anticoagulants), and drugs to stop bleeding (antifibrinolytics)
- High blood pressure
- High body mass index (BMI)
Contact Information
service@vejthani.com






















